Teladoc: Saving Lives or Just a Dime?
Teladoc, the largest telemedicine provider in the U.S., is on a mission to transform how patients receive health care.
Teladoc, the largest telemedicine provider in the U.S., is on a mission to transform how patients receive health care.1 Through an online two-sided marketplace, Teladoc connects 13 million patients with ~3,000 licensed physicians to provide affordable consultations on demand via phone or video. 2
Why Telemedicine?
When people get sick, they have three broad options:
- Self-treatment: best for common, low-risk ailments like colds and mild fevers that can be treated without prescription drugs
- Emergency room / urgent care: best for most serious situations such as major accidents, high fevers, etc.
- See your physician: best for cases that lie in between the above two extremes
It seems the current system is set up for success, spanning the gamut from low to high acuity. However, many common symptoms blur the lines between these options. Is your chest pain a result of indigestion or is it an early sign of a blocked artery requiring surgery? You don’t want to go to the emergency room and risk a multi-thousand-dollar bill when a simple physician visit could suffice. Similarly, you don’t want to wait until next Tuesday for an appointment with your physician if a complex surgery may be required. What to do? Enter telemedicine.
How Does Teladoc Add Value for Patients and Physicians on its Platform?
Teladoc’s promise to patients is three-pronged: 3
- Unparalleled access & convenience: 24/7/365 access to a physician within 10 minutes of request
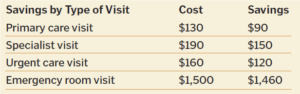
- Affordable care: ~$40 per consultation, significantly cheaper than existing alternatives (see Exhibit 1 below)
- Quality care: network of ~3,000 physicians is accredited by the NCQA (a well-established independent healthcare accrediting organization)
Exhibit 1: Savings Generated Using Teladoc vs. Alternatives 4
Similarly, Teladoc seeks to create value for physicians via: 5
- Increased flexibility: see patients whenever, from wherever
- Reduced overhead vs. in-person visit: fewer support functions required (receptionists, nurses, etc.)
- Increased patient volume: supplements slow daytime hours or allows a physician to earn extra money during nights/weekends
How Does Teladoc Deliver on its Customer Promise?
Teladoc has made several key decisions to be able to deliver on its promises, each with different tradeoffs:
All consultations are provided via video or phone. 6 First and foremost, this greatly increases access and convenience for patients vs. an in-person visit. Further, physician overhead costs are reduced, but critics would note that IT investments are still required. 7 However, phone/video consultations pose added risk for physicians, who are forced to make decisions with less information than a traditional in-person visit. 8 Given a doctor-patient relationship is established upon a single phone consultation, physicians are exposed to malpractice risk if their recommendation proves unsuitable. 9 To mitigate malpractice risk, Teladoc explicitly states that it only treats non-emergent conditions. 10
Physicians are contractors. 11 Pros include flexibility for physicians, ease of adding physicians to the platform, and eliminating the need for Teladoc to pay benefits to physicians. However, there could be adverse selection for lower-quality physicians who have poor reputations and thus require the supplemental patient volume. 12
Consultations are billed at a flat rate with no time limit. 13 Patients don’t feel like they are “on the clock”, thus they can take the time to get the care they need. However, this provides an incentive for physicians to speed through visits to maximize their revenue generation.
Patients cannot request physicians. 14 This preserves the homogeneity of demand, so physicians can have flexible hours while the system still maintains quick response times. The main drawback is that patients who use Teladoc as a replacement for primary care have little continuity of care. Additionally, the lack of repeat business combined with a flat consultation rate could lead to physicians providing lower quality care. 15
Is Telemedicine the Next Big Wave in Healthcare?
While using technology to increase access and convenience to health care while lowering costs seems compelling, skeptics question the efficacy of telemedicine. 16 In a world where continuity of care is constantly preached, are snippets of advice from rotating on-demand doctors good for us? Teladoc would argue that their services are a boon to the 62 million Americans who have inadequate access to primary care. 17 Regardless, the company should demonstrate the efficacy of its services through randomized controlled trials to establish credibility in both the medical and patient community.
There is an additional carrot looming down the road if telemedicine players can break through the trust barrier: partnering with insurers and acting as a gateway for the healthcare system. There’s huge value to be added by funneling patients to the most efficient site of care, vs. the status quo where patients routinely overconsume services to the financial detriment of insurers themselves. 18 Can telemedicine be the solution to ballooning healthcare costs?
Word count: 795
Sources:
- Teladoc, Form 10-K (filed May 26, 2016)
- Ibid
- Ibid
- CRAWFORD, MARK. “Technology Opens Promising Portals.”Health progress (Saint Louis, Mo.) 1 (2014): 18-21.
- Teladoc, Form 10-K (filed May 26, 2016)
- https://www.teladoc.com/how-does-it-work/
- CRAWFORD, MARK. “Technology Opens Promising Portals.”Health progress (Saint Louis, Mo.) 1 (2014): 18-21.
- http://www.modernhealthcare.com/article/20150221/MAGAZINE/302219981
- Scott, Ronald L. “TelaDoc Offers Telephone Consultations with Physicians.”
- https://www.teladoc.com/how-does-it-work/
- Teladoc, Form 10-K (filed May 26, 2016)
- Greene, Jan. “Emergency Physicians Among Specialties Seeking Part of the Telemedicine Pie.”Annals of Emergency Medicine 3 (2016): A20-A23.
- https://www.teladoc.com/frequently-asked-questions/
- Ibid
- http://www.modernhealthcare.com/article/20150221/MAGAZINE/302219981
- Greene, Jan. “Emergency Physicians Among Specialties Seeking Part of the Telemedicine Pie.”Annals of Emergency Medicine 3 (2016): A20-A23.
- Teladoc, Form 10-K (filed May 26, 2016)
- Petersen, Laura A., et al. “Nonurgent emergency department visits: the effect of having a regular doctor.”Medical care 8 (1998): 1249-1255.



I love this article! It’s a very clear, concise and structured overview of how we can think about telemedicine in our health system.
I completely agree that teledoc should run randomized control trials and cost studies in each of its services to assess its impacts. Unfortunately, healthcare is a very risk averse business that lends itself to very slow progress in the face of complex challenges. The only way to mitigate that is to expose uncertainties as vigorously as possible.
In teledermatology, for example, the American Academy of Dermatology and other prominent academic journals has published a number of trials looking at multiple telemedicine approaches for each of a large number of dermatologic diseases. For example, there have been trials looking at using DSLR camera images of microscope slides for remote cytology analysis (1), using contact immersion dermoscopy images for remotely assessing pigmented skin cancer lesions (2), and using DSLR camera images for remotely assessing non-pigmented skin cancer lesions (3). There have also been many studies looking at the costs of each of these programs (4).
I hope teledoc publishes similar studies of their own, because if their model is superior to what’s out there and they can reveal that through sound studies, that would be enormously beneficial to the field with growth and adoption of their models.
1.) Durdu, M. and Harman, M. (2016), Diagnostic value of telecytology in tertiary teledermatological consultation: a retrospective analysis of 75 cases. Int J Dermatol, 55: e392–e398. doi:10.1111/ijd.13219
2.) Erin M. Warshaw, Frank A. Lederle, Joseph P. Grill, Amy A. Gravely, Ann K. Bangerter, Lawrence A. Fortier, Kimberly A. Bohjanen, Karen Chen, Peter K. Lee, Harold S. Rabinovitz, Robert H. Johr, Valda N. Kaye, Sacharitha Bowers, Rachel Wenner, Sharone K. Askari, Deborah A. Kedrowski, David B. Nelson, Accuracy of teledermatology for pigmented neoplasms, Journal of the American Academy of Dermatology, Volume 61, Issue 5, November 2009, Pages 753-765, ISSN 0190-9622, http://dx.doi.org/10.1016/j.jaad.2009.04.032.
3.) Erin M. Warshaw, Frank A. Lederle, Joseph P. Grill, Amy A. Gravely, Ann K. Bangerter, Lawrence A. Fortier, Kimberly A. Bohjanen, Karen Chen, Peter K. Lee, Harold S. Rabinovitz, Robert H. Johr, Valda N. Kaye, Sacharitha Bowers, Rachel Wenner, Sharone K. Askari, Deborah A. Kedrowski, David B. Nelson, Accuracy of teledermatology for nonpigmented neoplasms, Journal of the American Academy of Dermatology, Volume 60, Issue 4, April 2009, Pages 579-588, ISSN 0190-9622, http://dx.doi.org/10.1016/j.jaad.2008.11.892
4.) April W. Armstrong, Julie Wu, Carrie L. Kovarik, Marc E. Goldyne, Dennis H. Oh, Karen C. McKoy, Alison M. Shippy, Hon S. Pak, State of teledermatology programs in the United States, Journal of the American Academy of Dermatology, Volume 67, Issue 5, November 2012, Pages 939-944, ISSN 0190-9622, http://dx.doi.org/10.1016/j.jaad.2012.02.019.
I should clarify that, thinking twice, an RCT would probably not be a feasible trial method to use for telehealth program assessment, but that’s a minor point. A similar study like a prospective control trial would be applicable here. But same concept.
Thank you for this post.
You ask that “Can telemedicine be the solution to ballooning healthcare costs?”. While I don’t have an answer to this question, I believe that telemedicine has a long way to go before it can become an effective mode of providing healthcare. For example, what if the patient who has already been seen by a doctor and advised a series of tests and gets them done only to discover that they were not needed in the first place because of a miscommunication between the doctor and patient while on videoconference? I personally feel that telemedicine is mainly a public health tool so that you can reach out to remote populations with basic diagnoses but the real checks and treatment will continue to happen live, and perhaps that’s a good thing.
Another consideration is how safe are the patient video-calls and health records? If you see this – https://krebsonsecurity.com/2016/10/europe-to-push-new-security-rules-amid-iot-mess/ – I fear that unless telemedicine providers beef up their systems so that patient data is extremely secure from hackers, the trust in telemedicine provision will never be built.
Thanks for writing about this! I wrote briefly about telemedicine in relation to One Medical and how they have added such features to their services. However, adding to Saurav’s skepticism above, I’m not sure if this can help ballooning healthcare costs, especially with the lack of continuity of care since patients cannot choose their doctors. I think there are opportunities to combine telemedicine with primary care services in the ways that One Medical is doing. Perhaps Teladoc should actually expand and have regular primary care centers to compete with a company like One Medical.