Supply Chain Management – A Matter of Life and Death

Could Supply Chain Management be the best Cure for Medical Errors in the US?
Killer Medical Errors
The United States spends more on health care than any other nation in the world, but it does not enjoy commensurate benefits in health outcomes. For example, the US spends $9,237 per capita on health care compared to $3,749 in the UK. Despite this, US life expectancy is 79.1 years, whilst UK life expectancy is 80.9 years [1]. Medical errors are estimated to be the third leading cause of death in the US [2].

Can supply chain management save us?
Improving visibility through digitization of the supply chain has the following potential benefits [5]:
- Better monitoring of health outcomes of individual patients
- Efficient and comprehensive product recalls in the event of medical device defects
- Cost effective and efficient inventory management
- High quality information on safety and efficacy of medical devices to inform future device innovations
- Federal oversight of health system performance in different regions
- Greater understanding of patient outcomes for individual disease states
With hospital payments moving from “fee-for-service” to “value based”, all hospitals should consider digitalizing the supply chain.
New federal laws
The ONC is the federal agency charged with supporting digitization of medical records to reduce medical errors and reduce. In 2016, 95% of hospitals had “meaningful” use of electronic health records (EHRs) [6]. The FDA, which regulates drugs and medical devices in the US has forced medical device companies to add unique identifiers (UDIs) to medical devices so that devices are traceable in the event of product recalls. However, FDA still does not require hospitals to track UDIs on EHR systems so many do not record them [4].
The Bringham and Women’s Hospital leads the way
Bringham and Women’s Hospital (BMH) in Boston have seized the opportunity to create efficiencies in their supply chain and improve traceability and safety outcomes. They have employed EHR systems to record UDIs, giving them a competitive advantage over other hospitals. However, for patients to be tracked longitudinally through different procedures, different providers and different geographies, most experts agree that UDI information needs to exist with insurance claim data [7]. They have now begun a pilot study into a process for transferring the UDI data to insurance claim forms [7].
In the medium term, the BMH can leverage patient data to use in their research programs to determine which devices work best in which patients [7]. This data will inform procurement plans for the BMH in the future, giving them a clear competitive advantage over other hospitals.
Data security
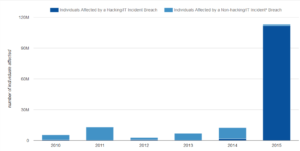
This strategy is not without its risks. The major potential concern with a move to digitalization is hacking. There has been a huge uptick in hacking incidents recently. The BMH will need to ensure it is taking every precaution to prevent leakage of protected health information of individuals.
Does a digitalized supply chain hold the key to solving other factors for premature death?
Social and environmental factors are now recognized as a major root cause of premature death in the US. This is illustrated best by the truly shocking statistic that there is a 20 year age gap between the life expectancy of men living in the most and least affluent areas of Baltimore, Maryland [9]. The BMH Center for Community Health and Health Equity was set up to tackle the problem of health inequity. In their 2016 Needs Assessment, one major factor listed was food insecurity [10]. The BMH could use a digitalized supply chain to provide healthy, nutritious food to these at-risk communities to improve patient outcomes. Boston Medical Center has already begun providing healthy, nutritious food to patients, tailored to their medical needs in what have been dubbed “food pharmacies” [11].
The big questions
Will the BMH prove that the cost and patient care benefits are worth the investment in a fully visible, digitalized supply chain? Can they keep patient data safe in the process?
Word count: 798 words
References
[1] Dieleman, J. et al. Evolution and patterns of global health financing 1995-2014. Lancet (2017).
[2] Makary, M. A. & Daniel, M. Medical error-the third leading cause of death in the US. BMJ: British Medical Journal (Online) 353, (2016).
[3] Fee-for-Service Still Dominates in United States. Available at: https://www.medscape.com/viewarticle/860003. (Accessed: 12th November 2017)
[4] Barlas, S. FDA Flags Inconsistent Hospital Reporting Of Medical Device Problems: Hazy Reporting Rules Beget Confusion. Pharmacy and Therapeutics 42, 97 (2017).
[5] Snowdon, A., Alessi, C., Visibility: The new value proposition for health systems. World Health and Innovation Network (2017).
[6] Office of the National Coordinator for Health Information Technology. ‘Hospital Progress to Meaningful Use by Size, Type, and Urban/Rural Location,’ Health IT Quick-Stat #5. dashboard.healthit.gov/quickstats/pages/FIG-Hospital-Progress-to-Meaningful-Use-by-size-practice-setting-area-type.php. (Accessed: 12th November 2017).
[7] Weissman, J. S., Krupka, D. C., Zerhouni, Y., Landman, A. & Wilson, N. Transmitting the UDI from the Point of Use to Insurance Claims: Changes in Workflows and Information Systems May 2017. (2017).
[8] Office of the National Coordinator for Health Information Technology. ‘Breaches of Unsecured Protected Health Information,’ Health IT Quick-Stat #53. dashboard.healthit.gov/quickstats/pages/breaches-protected-health-information.php. (Accessed: 12th November 2017)
[9] Marmot, M. The health gap: the challenge of an unequal world. The Lancet 386, 2442–2444 (2015).
[10] Community Health Needs Assessment. Available at: http://www.brighamandwomens.org/About_BWH/communityprograms/CHNAReports.aspx. (Accessed: 12th November 2017)
[11] Boston Medical Center makes healthy food part of patients’ medical care. AHA News Available at: http://news.aha.org/article/171013-boston-medical-center-makes-healthy-food-part-of-patients-medical-care-. (Accessed: 12th November 2017)



I think you raise a really important point that there is potential to improve patient outcomes through an increasingly data-driven approach to healthcare, but that cost and risk barriers to implementation exist and must be overcome. It seems like there is a bit of a chicken-and-egg conundrum because data is necessary to create the transparency to enable more value-based payments, which could save the healthcare system money by eliminating extraneous procedures / medicines / devices incentivized by fee-for-service and third-party (insurance) payment models. It also has the potential to reduce medical errors, and consequently costs. However, on top of the financial barriers and increased risk of holding more and more patient health information, there are numerous challenges associated with subverting traditional models. For example, with the implement of EHRs, providers have to spend more and more time on computers, rather than with patients. Nonetheless, the healthcare ecosystem is clearly moving in this direction, and ultimately all players must rely on data to justify treatment decisions. Fortunately, a number of mechanisms are in place – like the Health Insurance Portability and Accountability Act (HIPAA) to protect patient data. Moreover, as benefits are proven by early adopters like BMH, the business case will be impossible to ignore.
Professor Emeritus, this is a great initiative from Bringham and Women’s Hospital. Several providers (hospitals) around the world are working towards the development of an outcome-based valuation approach that allows a better allocation of resources towards.
The concern you bring about the costs versus benefits of the value based approach is a common issue among hospitals. Hospitals around the world are now taking the first but there is already significant evidence of success. Karolynska Institute, in Sweden, is a good implementation example, with proven better outcomes and cost savings.
To ensure that BWH follows the same success path as other providers, it is crucial to ensure BMH is 1) measuring the right metrics and 2) have the appropriate digital and organizational capabilities. Given the level of disruption that this new approach brings, I would recommend BMH to engage with ICHOM, a non-profit organization focused on defining standard sets and measure outcomes.[1]
These disruptive transformations are not easy and affect patients, physicians, and all support teams. Given that, it is crucial to ensure that BWH has the best process possible.
—
[1] ICHOM, “How to measure”. Retrieved from: http://www.ichom.org/, accessed on November 2017.